A friend of the family had recently brought her aunt to see me for treatment. She told me that she had Parkinson's Disease along with shoulder pain. I accepted to treat her with some hesitancy because I thought this would be a difficult issue. However, as soon as I treated her, everything just seemed to flow smoothly. We were seeing each other for a period of five non-consecutive sessions for two and half weeks.
My friend's aunt whom we will address as "Mrs. Patel," was 77-years old and was visiting her family from London, England. She was diagnosed with Parkinson's Disease in 1991. However, her main complaint was her shoulder pain that resulted from an accident during yoga practice which happened a long time ago.
After seeing how Mrs. Patel was unable to move her arm overhead (and only to the level of her collarbone forming a ninety degree angle), I immediately remember seeing this as frozen shoulder because of my past clinical experience. The pain quality ranged from dull and achy to sharp and stabbing. The pain was made worse with cold air emitted from central air conditioning to ingestion of cold foods. Her surgeon back in England did whatever he or she could to do to fix the problem after the accident. After the surgery, she was unable to move her arm. Furthermore, the surgeon had said that there was a piece of bone from the shoulder that got chipped off and was circulating inside the shoulder joint; thus making the shoulder pain even worse.
In regards to her Parkinson's Disease, it was heartbreaking to see. She had a shuffling gait while walking. She would clutch onto the side-railings with both hands to walk up and down a flight of stairs. Her body frame was frail and thin. Her visage looked very haggard and looked very tired. During the inquiry, she would often speak in a low tone of voice and she felt like sleeping all the time. All the muscles in her body felt very rigid and tense. She was on ten different medications; nine out of ten of them were for Parkinson's Disease and one of them was for bone and joint care.
In addition to that, Mrs. Patel said that the tremors in her hands were exacerbated with emotional and mental stress. One of her medications for Parkinson's was making her constipated; her stools were too dry and were happening once every day. Other signs and symptoms consisted of heavy eyelids and burning sensation in the eyes, vertex headaches, pain upon breathing, and lower back pain. Her pulse was thin, rapid, long and palpable at all three depths. The liver position as well as both kidney positions was very vacuous. While I was examining her pulse, Mrs. Patel and her niece mentioned that she had acupuncture done while she was on a cruise ship. Mrs. Patel said that the other acupuncturist said her liver and kidneys were very weak. It brought a smile to my face to know that there was someone in our field that I can concur with. While examining her tongue, the body was short and thin. The color of the tongue body was light red and the coating of the tongue was thin and white. After examining everything that I found, her diagnosis was "cold painful obstruction" (also known as Han Bi Zheng) and "wasting syndrome" (also known as Wei Zheng). Her pattern was internal wind due to systemic qi and yin vacuity and localized qi and blood stasis.
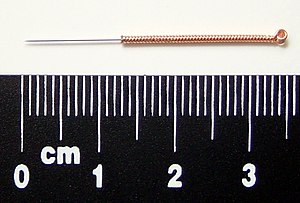
During the first treatment, getting her to come onto the table was difficult since I didn't have a step stool available at the time so I lifted her onto it. The first set of needles that went in the right shoulder was inserted into the local points and ashi points. Then I inserted needles into Zu San Li (ST-36), San Yin Jiao (SP-6), and Rang Gu (KID-2) for the qi and yin vacuity that was related to her Parkinson's. Next I used direct moxibustion on Qi Hai (CV-6) to help treat her fatigue using three cones. Also I manipulated the needles by hand using the reduction method to release the stagnated proteins her right shoulder and using the supplementation method to address the metabolic vacuities. After thirty minutes of needle retention and manipulation, I took out the needles and used pole moxibustion over her right shoulder. However, I used it in a way that was only taught to me by one my big influencing teachers. I took a paper towel, draped it over the right shoulder (the deltoid), and started tapping the lit end of the moxa pole onto the paper towel. This technique (which is not taught in TCM schools in the US) is much more powerful because the heat from the moxa penetrates deep to the tissues. The last part of the treatment involved tui na (medical massage) onto the shoulder.
This approach I used was the same approach I used in the other treatments that followed with a few modifications such as needle-head moxa over the right shoulder. After her first session was over, Mrs. Patel felt like her vitality had returned back. We continued treatment four more times. After she left my office after our first session with her niece, I noticed that Mrs. Patel was no longer walking like a frail, ill woman. She was walking like a twenty year old. I was worried thinking that the next time I'd see her she would be back to square one. However, when she came for her second session, she was walking the same way as she did after her first session. She did feel some level of trepidation walking up and down a flight of stairs. Despite that, she was still walking smoothly.
After our last session together on August 21st, Mrs. Patel's could now lift her right arm to a one-hundred and twenty degree angle. That showed tremendous amount of improvement than when I saw her for her first session. Unfortunately, with the constraints of time, we couldn't see each other anymore since she had to leave for London the next day. Before Mrs. Patel left, I gave her the name of an acupuncturist and an herbalist in London.
Billy Shonez Singh is a licensed acupuncturist and a board certified Chinese herbalist by the NCCAOM. He is currently practicing in Commack, NY. His primary focus with East Asian medicine is stress, pain management, diabetic complications, and treating chemotherapy side-effects
Billy Singh, L. Ac. is a graduate of
New York College of Traditional Chinese Medicine's Herbal Certificate Program for Acupuncturists.










![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=1d183d3c-0314-47a7-b845-ef63dc4ff3f7)

![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=8b4a3251-285b-4710-8ea6-78f1a1fb12d4)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=c6f99c15-7434-48b2-9127-ae97ae161f5f)

![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=b80124be-955b-4b06-a9a5-5ba40fef227c)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=7b2f351c-e0d6-46d6-bc9d-330687e1d943)